Improving Intranasal Naloxone Delivery Using Excipients in a Tissue Model
- TR Number: 1092
- Authors: Veronica F. Blanco, Garima Sinha, Christian Wells, Amy Druschitz, Kate McEvoy, Dharshana Padmakshan Croda
- Keywords: EpiNasal (NAS-100), intransal drug delivery, avoidance of first pass metabolism, excipients, dodecyl-ß-D-maltoside (DDM), n-dodecyl phosphocholine DPC, Polysorbate 80, naloxone hydrochloride, nasal toxicity, CellTiter Blue, alkylphosphocholine, modulation tight junctions, long chain alkylmaltoside, disrupt lipid packing
- Materials Tested: dodecyl-ß-D-maltoside (DDM), n-dodecyl phosphocholine DPC, Polysorbate 80, naloxone hydrochloride
Purpose: Intranasal delivery is an attractive route for systemic drug administration due to its non-invasiveness, rapid onset, avoidance of first pass metabolism, and patient comfort and compliance. However, drug absorption through the nasal mucosa faces several formulation challenges, including low permeability for hydrophilic and high-molecular-weight drugs, rapid mucociliary clearance, and enzymatic degradation in the nasal mucosa. Strategies to enhance nasal drug transport, such as the use of permeation-enhancing excipients, are therefore of significant interest in formulation development.1,2 This study aims to investigate the effect of n-dodecyl-ß-D-maltoside (DDM), n-dodecylphosphocholine (DPC), and Polysorbate 80 on the permeation of Naloxone Hydrochloride, a model small molecule drug, across a physiologically relevant 3D human nasal tissue model (MatTek EpiNasal™).
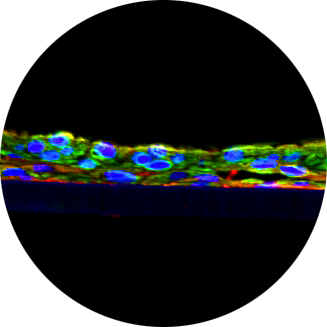
Methods: The permeability of naloxone hydrochloride was evaluated over 4 hours using the EpiNasal™ 3D in vitro nasal tissue model (NAS-100-BETA, MatTek Corporation, Ashland, MA). Tissues were stabilized for 24 hours in maintenance medium (NAS-100-MM) in a humidified incubator at 37 °C and 5% CO₂. For the permeation study, the medium was replaced with prewarmed 1× phosphate-buffered saline (PBS). Four groups were tested in parallel: (1) control with 200 μL of 10 mg/mL naloxone hydrochloride in PBS, (2) 0.1% DDM (Avanti), (3) 0.1% DPC (Avanti), and (4) 0.5% Super Refined Polysorbate 80, all formulated with 10 mg/mL naloxone hydrochloride in 1× PBS. Each formulation was applied to the apical side of tissue inserts and run in triplicate. Permeability was assessed by sampling the basolateral compartment containing 1 mL prewarmed PBS as receiver fluid at set time points. Naloxone concentrations were quantified using an Agilent 1260 HPLC with a Poroshell 120 Phenyl-Hexyl column (3.0 × 100 mm, 2.7 µm). The mobile phase was 0.1% formic acid in 10 mM ammonium formate (A) and methanol (B), with 25% B isocratic elution at 0.6 mL/min and a 4 min run time. Detection was at 281 nm using a UV detector, with a 10 µL injection. Cytotoxicity was assessed 24 hours post-treatment using the CellTiter-Blue® Cell Viability Assay (Promega). Tissues were incubated with reagent for 2 hours at 37 °C, and absorbance was recorded at 570/600 nm. Viability was expressed as a percentage of untreated controls. Statistical analysis used one-way ANOVA with Dunnett’s post hoc test (*p ≤ 0.05).
Results: The cumulative permeation of naloxone hydrochloride across EpiNasal™ tissue over 4 hours is shown in Figure 1. Both DPC and DDM significantly enhanced naloxone permeation compared to the control group (p < 0.001). In contrast, Super Refined Polysorbate 80 at 0.5% did not result in a significant increase in permeation. Similarly, calculated flux and apparent permeability values (Table 1) were statistically highest for DDM (24.67 µg/cm²/h, Papp = 24.67 × 10⁻⁴ cm/s) and DPC (23.21 µg/cm²/h, Papp = 23.21 × 10⁻⁴ cm/s), while SR Polysorbate 80 showed values comparable to the control. Cell viability analysis at 24 hours (Figure 2) revealed no detectable cytotoxicity in any treatment group, with all formulations maintaining excellent viability, above 85%. The enhanced performance of DDM and DPC is consistent with their membrane-active mechanisms. DDM, a long chain alkylmaltoside, increases permeability primarily by disrupting lipid packing within the apical membrane, thereby enhancing transcellular drug transport. As shown in a prior study,3 DDM’s 12-carbon chain provides an optimal balance of surfactant activity and biocompatibility, where shorter chain analogs (e.g., C8) show reduced efficacy, while longer chains (C14–C16) may cause excessive disruption and toxicity. Moreover, DDM does not irreversibly damage tight junctions but temporarily disrupts membrane microdomains, facilitating drug passage without prolonged epithelial compromise4. N-dodecylphosphocholine (DPC), is a C12 alkylphosphocholine structurally related to lysophospholipids. It has been shown to enhance paracellular permeability by modulating tight junctions, as demonstrated in Caco-2 epithelial monolayers where it reduced transepithelial electrical resistance (TEER) and increased permeability of hydrophilic markers, without inducing substantial cytotoxic effects5.
Conclusion: Intranasal delivery enables rapid, non-invasive systemic drug administration but faces barriers like mucociliary clearance, enzymatic degradation, and low epithelial permeability, necessitating optimized formulations and permeation enhancers6,7. In this study, n-dodecyl-β-D-maltoside (DDM) and n-dodecylphosphocholine (DPC) both increased the permeation of naloxone hydrochloride across the EpiNasal tissue model without compromising cell viability. These findings are consistent with known mechanisms of action for long-chain surfactants, which transiently disrupt membrane structure and enhance drug diffusion while maintaining epithelial integrity. Super Refined Polysorbate 80, on the other hand, did not improve permeability at the tested concentration of 0.5%. Although it is widely used in pharmaceutical formulations, it may require higher concentrations or co-formulation strategies to exhibit meaningful permeation-enhancing effects in nasal applications. Overall, these results support the utility of DDM and DPC as effective excipients for enhancing intranasal delivery of small molecules like naloxone, and they underscore the need for excipient-specific optimization during nasal formulation development