RECONSTRUCTION OF NEW ORGANOTYPIC 3D HUMAN SMALL INTESTINE TISSUE MODEL FOR DRUG SAFETY AND TOXICITY.
- TR Number: 750
- Keywords: BCRP, brush border membrane, Caco-2, CYP3A4, Cytokeratin-19, Cytokeratin-8, efflux drug transporters, Gro-α, IL-8, Kerckring folds, Lucifer yellow leakage, MDR-1, MRP-1, MRP-2, Mucin-2, Mucous secretory granules, P-glycoprotein, Small intestine, TEER, Villin
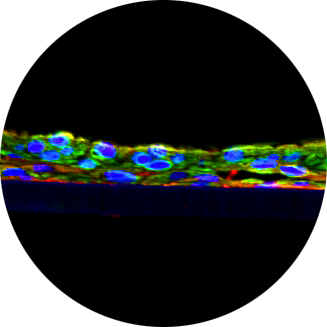
The epithelial lining of the gastrointestinal (GI) tract is a gatekeeper for entry of orally ingested nutrients and xenobiotics including medicaments. The small intestine has a well organized structure containing proliferative cells which migrate along the crypt-villi axis and differentiate into functionally mature epithelial cells. Currently, the most common in vitro model utilized for study of drug absorption in the small intestine is a 2-dimensional cell culture model cultured using the colon carcinoma cell line, Caco-2. These cells differentiate into monolayers of polarized enterocytes that are connected by tight junctions, but lack mucus-secreting goblet cells and show inter-passage inconsistency in the expression of drug transporters. Others have developed small intestine organoids which are not suitable for topical application of test articles. Here, we report the reconstruction of a human organotypic small intestine (SI) tissue model generated from primary human small intestinal (SI) epithelial cells that grow in tissue culture inserts using serum free medium. Normal (non-cancerous), human SI epithelial cells and myofibroblasts were expanded in monolayer culture and seeded on a microporous membrane containing a fibroblast-collagen-gel substrate to reconstruct 3-dimensional organotypic SI tissues. Tissue morphology, surface biomarker expression, and ultrastructural features of the SI model were characterized by H&E staining, immunohistochemistry, and transmission electron microscopy, respectively. Basal cell proliferation markers, cytokeratins (CK), mucin, and brush border membrane formation were monitored. Drug transporter expression was checked by RT-PCR. Tissue responses to inflammatory stimuli were examined following TNF-α exposure. Analysis of the SI tissue revealed: 1) wall-to-wall growth of the epithelial layer, 2) columnar epithelial cell morphology similar to that of native SI tissue, 3) expression of Mucin-2 (MUC-2), CK19, and villin at the surface of the epithelium, and 4) formation of brush borders and tight junctions. RT-PCR results showed expression of efflux drug transporter genes, MDR-1, MRP-1, MRP-2, and BCRP, and the metabolic enzyme, CYP3A4. Treatment of the Si tissue model with TNF-α induces a proinflammatory response by inducing the C-X-C chemokines such as IL-8 and GRO-α. In conclusion, the new human cell based 3D, SI tissue model will likely serve as a valuable tool to evaluate safety and adsorption of pre-clinical therapeutic drug candidates intended for oral administration as well as preclinical study of intestinal mucosal inflammation, microbiomes, and microbial infection mechanisms in the gastrointestinal microenvironment.