ANTIMICROBIAL BARRIER OF AN IN VITRO ORAL EPITHELIAL MODEL.
- TR Number: 424
- Keywords: Beta-defensins, Buccal mucosa, Commensal bacteria, EpiOral, Extracellular matrix, Fusobacterium nucleatum ATCC 25586, GAPDH, Gram-negative bacteria, Human beta-defensin 1 (hBD1), Human beta-defensin 2 (hBD2), Human beta-defensin 3 (hBD3), IL-8, Keratin 13, Keratin 14, Microbial barrier , Normal human oral keratinocytes, ORL-100, Oral cavity, PAR 1, PAR 2, Pathogenic bacteria, Porphyromonas gingivalis, Proinflammatory cytokines , Rabbit polyclonal antibodies , Ribosomal phosphoprotein (RPO), Streptococcus gordonii, Toll like receptors 2 (TLR 2), Toll like receptors 4 (TLR 4)
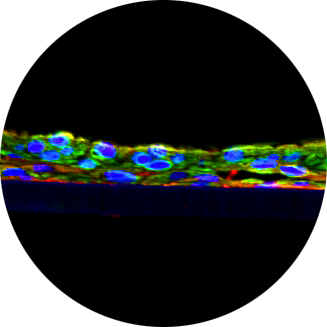
This study by researchers at the University of Washington demonstrated that Mattek’s EpiOral human buccal tissue equivalent has an in vivo-like antimicrobial barrier and is therefore a superior in vitro model of oral epithelia when compared to submerged monolayer cell cultures. Objective: Oral epithelia function as a microbial barrier and are actively involved in recognizing and responding to bacteria. In this study, the objective of researchers at the University of Washington was to examine Mattek’s EpiOral™, a tissue engineered model of buccal epithelium, for its response to oral bacteria and proinflammatory cytokines and compare the EpiOral tissue responses with those of a submerged monolayer cell culture. Design: The EpiOral tissue model was characterized for keratin and b-defensin expression. Altered expression of b-defensins was evaluated by RT-PCR after exposure of the apical surface to oral bacteria and after exposure to TNF-a in the medium. The EpiOral responses were compared to the response in traditional submerged oral epithelial cell culture. Results: The EpiOral buccal model showed expression of differentiation specific keratin 13, hBD1 and hBD3 in the upper half of the tissue; hBD2 was not detected. hBD1 mRNA was constitutively expressed, while hBD2 mRNA increased 2-fold after exposure of the apical surface to three oral bacteria tested and hBD3 mRNA increased in response to the non-pathogenic bacteria tested. In contrast, hBD2 mRNA increased 3—600-fold in response to bacteria in submerged cell culture. HBD2 mRNA increased over 100-fold in response to TNF-a in the EpiOral tissue model and 50-fold in submerged cell culture. Thus, the EpiOral tissue model is capable of up-regulating hBD2, however, the minimal response to bacteria suggests that the EpiOral tissue has an effective antimicrobial barrier due to its morphology, differentiation, and defensin expression. Conclusions: The EpiOral oral mucosal model is differentiated, expresses hBD1 and hBD3, and has an intact surface with a functional antimicrobial barrier.